Thomas C. Pitts, M.D.
Director of Neurology – Hudson Medical
Diplomate of the American Board of Psychiatry and Neurology with Special Qualifications in Clinical Neurophysiology
Added Qualifications in Headache Medicine – National Headache Foundation
Certified Multiple Sclerosis Specialist – Consortium of Multiple Sclerosis Centers
Myasthenia Gravis Foundation of America Partner Provider
Alumni – Columbia University College of Physicians Surgeons
Alumni – Wright State University Boonshoft School of Medicine
Consent: Consent was obtained from the patient’s power of attorney in this case as the patient was critically ill, intubated, and sedated during this time period.
Disclosures: There is no financial support associated with this study. Medication is provided to the institution for free by Alexion Pharmaceuticals subsequent to the approval of an emergency investigational new drug application by the FDA. The author is a member of the Alexion speaker’s bureau.
Key words: Eculizumab, Soliris, Coronavirus, Covid-19, Complement, ARDS, Acute Respiratory Distress Syndrome
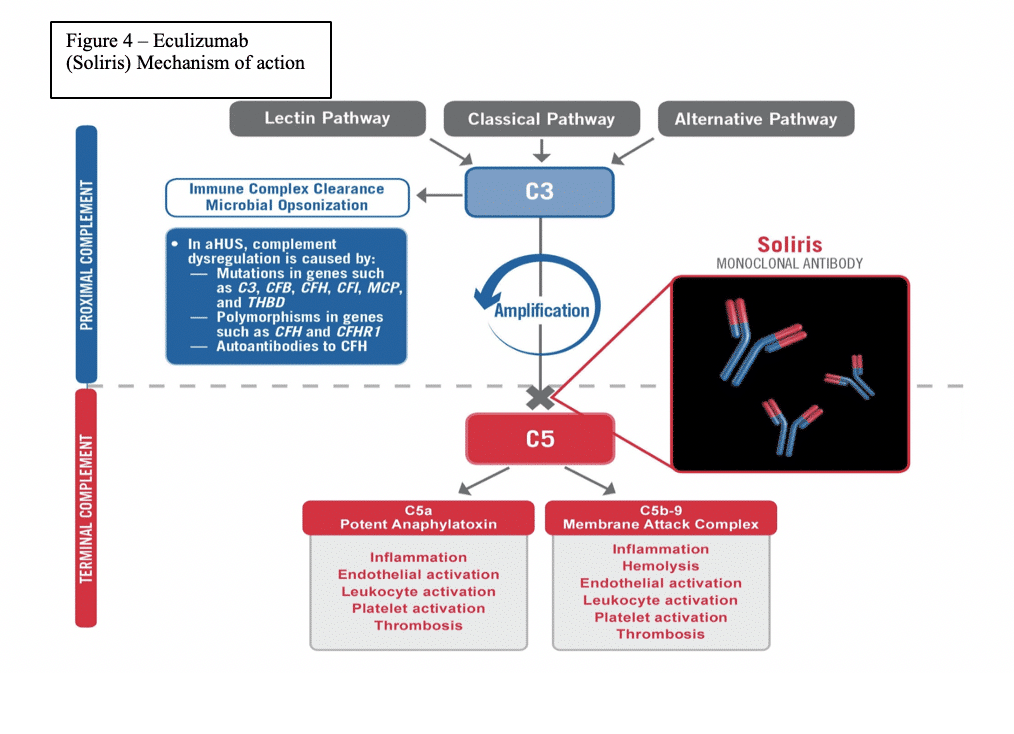
Abstract: Covid-19 has spread rapidly throughout the world causing widespread injury, and death. While this virus is the provocateur, it is often the patient’s own disproportionate immune response which likely deals the most devastating (and often fatal) damage. The Membrane Attack Complex (MAC) is a primary mediator of this catastrophic, immune mediated, end organ damage and is formed by the various components of the distal complement (C5-C9). The MAC is ordered to form and attack when C1q, a surveillance component of the complement system, surveys the antigen and calls upon its destruction even if the involvement of the MAC causes the devastating destruction to the end organ within which the virus exists (i.e the lungs). This mechanism has been shown to be a cause such damage in other types of coronaviruses. In the SOLID-C19 compassionate use study, Soliris (Eculizumab) is being used to modulate the activity of the distal complement by preventing the formation of the MAC. By modulating this portion of the immune response, mortality can be halted while the patient has time to recover from the virus with supportive medical care. The proximal complement is left intact. The MAC’s primary role is to combat certain encapsulated bacteria; thus, its inhibition should stop immune mediated end organ destruction while not hindering viral fighting components of the immune system. This case demonstrates effective targeting of the distal complement to halt catastrophic complement mediated lung damage and acute respiratory distress syndrome (ARDS) in an intubated, covid-19 positive patient who was on hydroxychloroquine chronically for lupus in life-threatening condition.
Case Presentation: A 44-year-old female respiratory therapist for an assisted living facility who was taking hydroxychloroquine and mycophenolate mofetil chronically for Lupus called her rheumatologist on March 12th2020 concerned about a possible Lupus flare complaining of intermittent fever, cough, and generalized myalgias including chest discomfort when breathing. The rheumatologist stopped her mycophenolate mofetil and started her on 40mg po daily prednisone with a 12-day taper at that time. On March 16th, 2020 the patient went to her primary care physician because these symptoms were becoming more frequent and bothersome, and she now reported dyspnea when laying supine. The patient even noticed some crackles when she listened to her own lungs. Rhonchi in the left upper lung were noted on physical exam. A rapid flu and urine test were normal. Chest x-ray showed left midlung disease. It was speculated that this could be a developing pneumonia and so doxycycline was started. She was sent to the emergency department for covid-19 testing and went home after the test, reportedly in no acute distress. She was told to quarantine for 14 days as she was exposed to covid-19 positive patients in the assisted living facility where she worked.
The patient subsequently reported to the emergency department on March 18th2020 with worsened dyspnea as well as lightheadedness. Electrocardiogram was normal. Chest x-ray showed mild to moderate bibasilar opacities. Her oxygen saturation was 88% during this evaluation on room air and she had a fever of 38.8 C. CT PE study was obtained and remonstrated the bibasilar opacities and was negative for pulmonary embolism. She was admitted to the hospital. That night she had worsening dyspnea and her fever rose to 39 C. She was intubated and transferred to the intensive care unit. At the time of intubation her blood pressure was 84/45 and her respiratory rate was 43/min. Repeat chest x-ray after intubation showed significant progression of the bilateral lung disease consistent with acute respiratory distress syndrome (ARDS). CRP at the time of intubation was 33.7. Flu and RSV were negative. The patient was started on piperacillin/tazobactam and norepinephrine by the medical critical care team.
While intubated, the patient continued to have desaturation of her oxygen. Her PaO2 was 71 while intubated and she had a generalized seizure. Her ventilator settings were adjusted and her SPO2 rose to 95%. A chest x-ray was again obtained which remonstrated findings consistent with severe ARDS with superimposed bilateral pulmonary edema. furosemide 40mg IV was given at that time. The patient was moved to a rotaprone bed and turned to the prone position as she continued to have intermittent desaturations while supine despite mechanical ventilation.
Certriaxone 2gm every 12 hours was ordered by the infectious disease team and piperacillin/tazobactam was discontinued. Azithromycin was also added. She remained on hydroxychloroquine and her steroids were stopped. Neurology was consulted who ruled out CNS disease and attributed the seizure to hypoxia. The patient’s husband and three children were reportedly brought into the quarantine area to see the patient as they were reportedly told that she may not recover from this illness.
The consulting Neurologist Dr. Eleina Mikhaylov, notified the author to see if she would qualify for the Soliris to Stop Immune Mediated Death in Covid 19 Infected Patients compassionate use study(SOLID-C19 – NCT04288713 clinicaltrials.gov). The author and Dr. Mikhaylov obtained consent from the patient’s husband to enroll the patient in the trial after local IRB and FDA eIND approvals were obtained. Eculizumab was sent to the facility emergently and was given at 10:30pm on 3/23/2020.
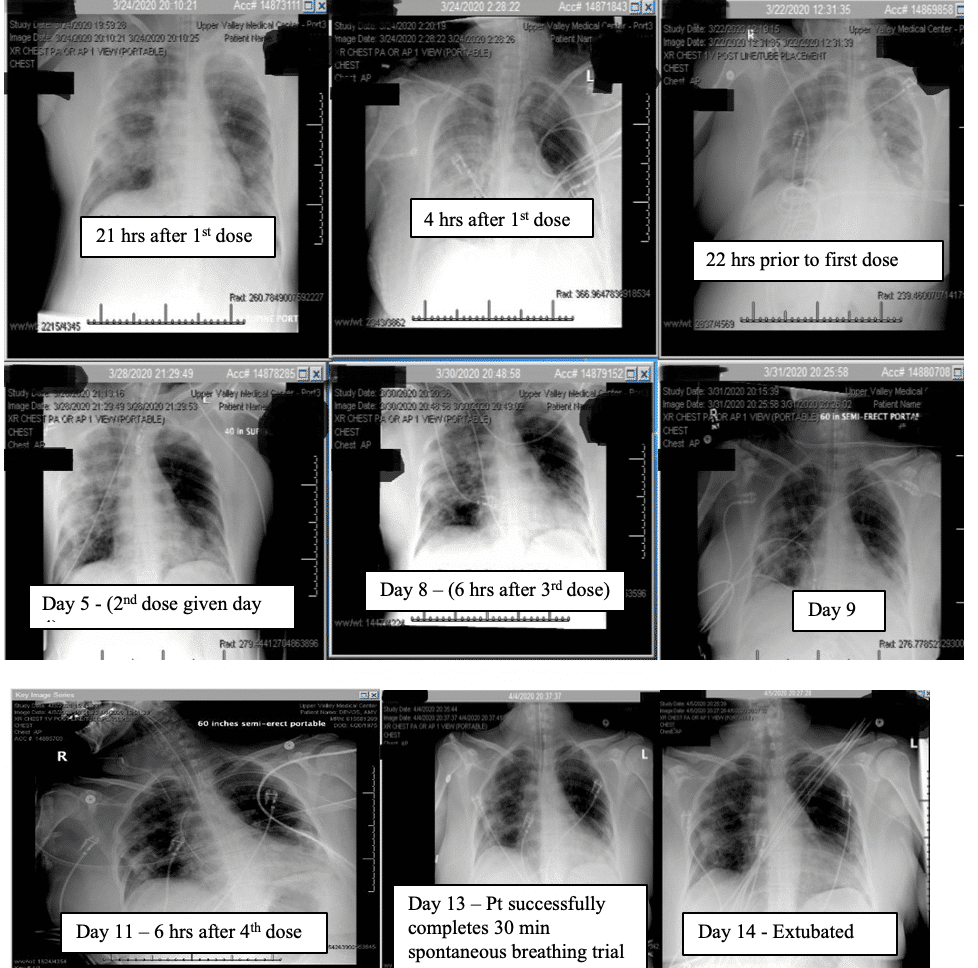
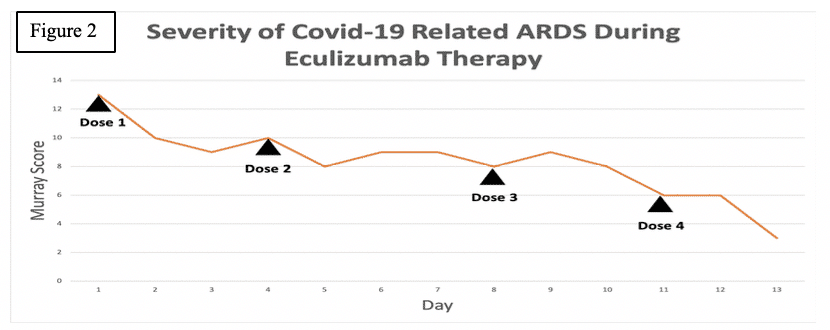
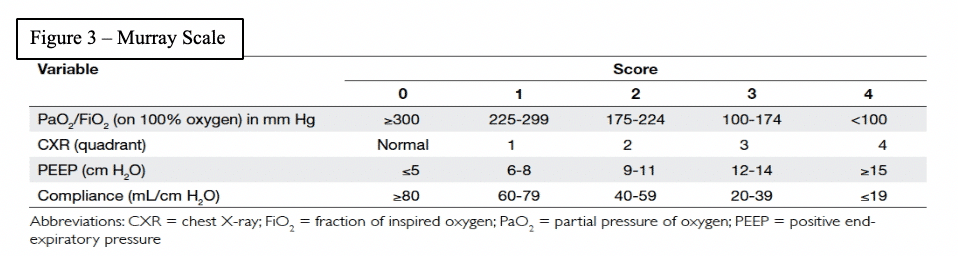
The patient’s Murray score was 13/16 prior to the first dose. She was given eculizumab 900mg IV over 35 minutes for each dose. Her Rocephin served as her meningococcal prophylaxis. The seroB and quadrivalent meningococcal vaccines were also administered.
Within 4 hours after the first dose of eculizumab her chest x ray improved, and her Murray score improved from 13 to 10. She had a daily improvement in Murray score except on March 27th 2020 when her endotracheal tube moved out of place while she was prone and had to be readjusted in which case her Murray score rose slightly but still remained lower than her pre-trial baseline. Another 900mg IV eculizumab dose was given 4 days after the first dose and, again, her chest x-ray improved. Her hydroxychloroquine was stopped on March 28th 2020 due to possible contribution to a normocytic anemia. Norepinephrine was discontinued on March 29th 2020 as her blood pressor stabilized. The patient was able to be adequately oxygenated in the supine position and her rotabed was discontinued on March 31st 2020. On April 2nd 2020 her third dose of eculizumab 900mg IV was given and her Murray score improved from 8/16 on April 1st 2020 to 6/16 recorded 7 hours after the third dose of eculizumab was given on April 2nd 2020. On April 3rd 2020 the medical critical care team started to wean the patient’s sedation (propofol, fentanyl, and midazolam). The patient passed a 30 spontaneous breathing trial and followed appendicular commands on April 4th 2020. Mechanical ventilation was continued to allow the sedation to fully wear off in preparation for extubation. The patient’s Murray score had decreased to 3/16, she was able to oxygenate in the supine position, remained afebrile, and did not require presser medications. She was successfully extubated on April 5th 2020. She was neurologically intact and even “face-timed” on the phone with family a few hours subsequent to extubation.
Discussion:Identifying the highest value approach for a patient is not always clear. While many efforts have been made to treat the virus itself in covid-19 patients, this case highlights the vital role of immunomodulation to halt the catastrophic complement mediated lung damage that occurs covid-19 related ARDS. Successful extubation was facilitated by modulation of this immune mediated damage and allowing the body’s normal anti-viral mechanisms to clear the virus (as with most coronaviruses that we regularly encounter) with supportive medical care. The implication is that the virus may not be as high value a target as its provoked immune response.
The author would point out that we as humans interact with coronaviruses on a daily basis. It is the likely the fact that because this covid-19 is unknown to our immune system it triggers C1q to initiate the overwhelming, disproportionate, and often lethal complement mediated immune response which directs the MAC against the virus and destroys the lungs and other end organs in the process.
This case is especially important because the patient also has lupus and a history of positive SS-B and ANA antibodies in her blood. It is well described that patients with autoimmune diseases may have exacerbations of their conditions in the setting of illness and immune activation (ie Myasthenia Gravis crisis with an infection or surgery) and it is plausible that this patient had to not only contend with the immunological onslaught provoked by the virus but also from her chronic autoimmune disease (especially as her mycophenolate mofetil and subsequently her hydroxychloroquine were stopped). It is also well described that immune mediated damage can continue long after the inciting infectious pathogen has been cleared from the body (i.e. viral or bacterial provoked Guillain-Barre syndrome leading to CIDP). In fact, while the patient tested positive for Covid-19 initially, her Covid-19 test drawn on the day of extubation was negative which shows that the immune mediated damage can continue after the virus becomes undetectable in the blood. It is important to note that we immunomodulate Guillian-Barre patients in this situation rather than trying to treat them with anti-viral medications as their misguided and overwhelming immune response is the primary cause of end-organ damage which is likely the case in Covid-19 mediated ARDS.
It is also critical to point out that the patient was intubated and almost died while on hydroxychloroquine chronically and did not clinically improve with the concomitant administration of azithromycin. It was not until eculizumab was delivered that the patient began to improve (see chest x-ray for hours after the first dose). The patient also continued to improve despite hydroxychloroquine being stopped by the infectious disease consultant due to a concern for anemia.
In a disease state for which certain data suggests 86%-97% of intubated patients with covid-19 related ARDS die, inhibition of the membrane attack complex with eculizumab was effective in saving this patient’s life and setting the stage for likely extubation. While this is compassionate use data in a single patient, the high mortality rate in the general covid-19 related ARDS population can feasibly serve as a “natural control.” In any event, this is an extremely promising therapeutic approach and merits further direct clinical implementation and study. This is especially true because, in the process of halting the catastrophic immune response, eculizumab does not inhibit viral fighting mechanisms. Eculizumab safety is substantiated in numerous studies as well as almost two decades of case studies for its four other FDA indications (AchR + generalized myasthenia gravis, atypical hemolytic uremic syndrome, paroxysmal nocturnal hemoglobinuria, and anti-AQP4 neuromyelitis optica). There are also several case studies citing the safety of eculizumab in pregnant patients. It is vital that we act promptly during this troubling time and facilitate the investigation of promising and possibly lifesaving therapies which have been proven safe for almost two decades. This is exceptionally true given the fact that ICUs and hospitals are, in many places, becoming overwhelmed and often in short supplies of invasive ventilators.
Summary –Distal complement inhibition preventing formation of the membrane attack complex and is associated catastrophic end organ damage is a promising and relatively safe approach in covid-19 related ARDS. This was demonstrated in this 44-year-old patient with concomitant lupus who was intubated and did not improve despite being on hydroxychloroquine chronically or with the addition of azithromycin. After the administration of eculizumab the objective data shows a clear and sustained clinical improvement and preservation of life. The patient was successfully extubated.
References:
- Gralinski LE1, Sheahan TP1, Morrison TE2, Menachery VD1,3, Jensen K1, Leist SR1, Whitmore A4, Heise MT4, Baric RS5. Complement Activation Contributes to Severe Acute Respiratory Syndrome Coronavirus Pathogenesis. Pubmed [Internet]. 2018 Oct [cited 2020 Apr 5]; [1 p.]. Available from: https://www.ncbi.nlm.nih.gov/pubmed/30301856
- Guang Sheng Ling, Greg Crawford, Norzawani Buang, Istvan Bartok, Kunyuan Tian, Nicole M. Thielens, et al. C1q restrains autoimmunity and viral infection by regulating CD8+ T cell metabolism. AAAS Science [Internet]. 2018 May [cited 2020 Apr 5]; [1 p.]. Available from: https://science.sciencemag.org/content/360/6388/558
- Skeptical Scalpel. Mortality of Covid-19 Patients on Ventilators. Physician’s weekly [Internet]. 2020 Mar [cited 2020 Apr 5]; [1 p.]. Available from: https://www.physiciansweekly.com/mortality-rate-of-covid-19-patients-on-ventilators/
- Richard J. Kelly, M.B., Ch.B., Ph.D., Britta Höchsmann, M.D., Jeff Szer, M.B., B.S., Austin Kulasekararaj, F.R.C.Path., Sophie de Guibert, M.D., Alexander Röth, M.D, et al. Eculizumab in Pregnant Patients with Paroxysmal Nocturnal Hemoglobinuria. NEJM [Internet]. Sep 2015 [cited 2020 Apr 5]; [1 p.]. Available from: https://www.nejm.org/doi/pdf/10.1056/NEJMoa1502950.
- Howard JF Jr, Utsugisawa K, Benatar M, Murai H, Barohn RJ, Illa I, et al. Safety and efficacy of eculizumab in anti-acetylcholine receptor antibody-positive refractory generalized myasthenia gravis (REGAIN): a phase 3, randomized, double-blind, placebo-controlled, multicenter study. Pubmed [Internet]. Dec 2017 [cited 2020 Apr 5]; [1 p.]. Available from: https://clinicaltrials.gov/ct2/show/NCT01997229
- Pittock SJ1, Berthele A1, Fujihara K1, Kim HJ1, Levy M1, Palace J, et al. Eculizumab in Aquaporin-4-Positive Neuromyelitis Optica Spectrum Disorder.Pubmed [Internet].Aug2019[cited 2020 Apr 5]; [1 p.]. Available from:https://www.ncbi.nlm.nih.gov/pubmed/31050279?dopt=Abstract
- C.M. Legendre, C. Licht, P. Muus, L.A. Greenbaum, S. Babu, C. Bedrosian, et al. Terminal Complement Inhibitor Eculizumab in Atypical Hemolytic–Uremic Syndrome. NEJM [Internet]. Jun 2013 [cited 2020 Apr 5]; [1 p.]. Available from: https://www.nejm.org/doi/full/10.1056/NEJMoa1208981
- Charles Parker, M.D. Eculizumab for Paroxysmal Nocturnal Hemoglobinuria. Lancet [Internet]. Jan 2009 [cited 2020 Apr 5]; [1 p.]. Available from: https://www.thelancet.com/journals/lancet/article/PIIS0140-6736(09)60001-5/fulltext
- Muppidi S, Utsugisawa K, Benatar M, Murai H, Barohn RJ, Illa I, Long-term safety and efficacy of eculizumab in generalized myasthenia gravis. [Internet]. Jan 2009 [cited 2020 Apr 5]; [1 p.]. Available from: https://www.ncbi.nlm.nih.gov/pubmed/?term=Muppidi%20S%5BAuthor%5D&cauthor=true&cauthor_uid=30767274